From early warnings to smarter ventilators, artificial intelligence is helping clinicians outpace ARDS, offering hope for more lives saved through personalized, data-driven care.
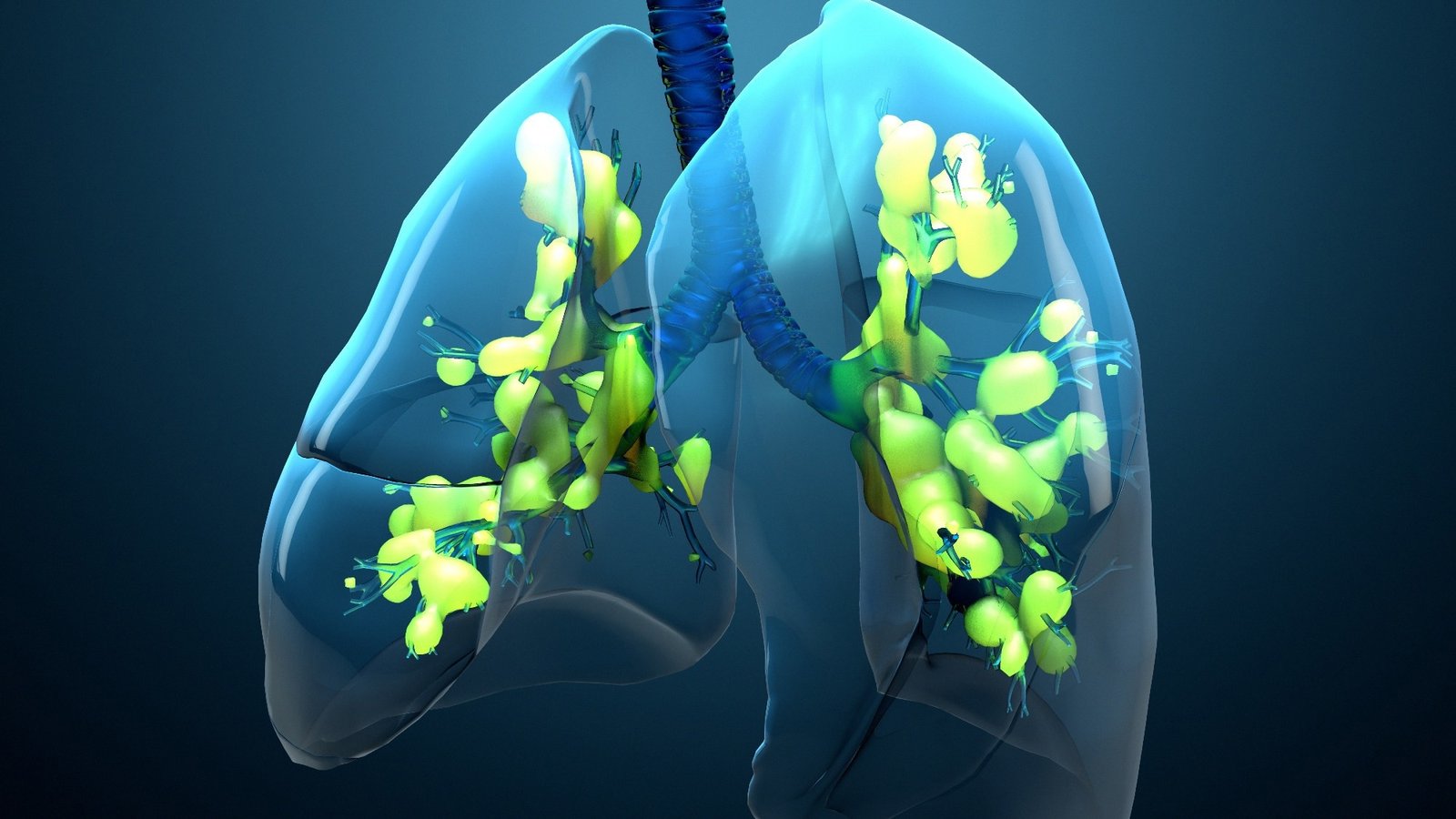
Review: Artificial intelligence and machine learning in acute respiratory distress syndrome management: recent advances. Image Credit: Design_Cells / Shutterstock
In a recent review published in the journal Frontiers in Medicine, a group of authors synthesized recent evidence on how artificial intelligence (AI) and machine learning (ML) enhance prediction, stratification, and treatment of acute respiratory distress syndrome (ARDS) across the patient journey.
Background
Every day, more than one thousand people worldwide enter an intensive care unit (ICU) with ARDS, and 35–45% of those with severe illness still die despite guideline-based ventilation and prone positioning. Conventional care works, yet it remains fundamentally supportive and cannot overcome the syndrome’s striking biological and clinical heterogeneity. Meanwhile, the digital exhaust of modern ICUs, continuous vital signs, electronic health records (EHRs), imaging, and ventilator waveforms has outgrown the capabilities of unaided human cognition. AI and ML are increasingly being explored as tools that promise to transform this complexity into actionable insight. However, as the review notes, external validation, generalizability, and proof of real-world benefit remain crucial research needs. Further research is needed to determine whether these algorithms actually improve survival, disability, and cost.
Early Warning: Predicting Trouble Before It Starts
ML algorithms already flag patients likely to develop ARDS hours and sometimes days before clinical criteria are met. Convolutional neural networks (CNNs) trained on chest radiographs and ventilator waveforms, as well as gradient boosting models fed raw EHR data, have been shown to achieve area under curve (AUC) values up to 0.95 for detection or prediction tasks in specific settings. However, performance varies across cohorts and model types. This shift from reactive diagnosis to proactive screening enables teams to mobilize lung-protective ventilation, fluid stewardship, or transfer to high-acuity centers earlier, a practical advantage during coronavirus disease 2019 (COVID-19) surges when ICU beds are scarce. The review highlights that combining multiple data types, clinical, imaging, waveform, and even unstructured text, generally yields more accurate predictions. Still, real-world accuracy remains dependent on the quality of the data and external validation.
Sharper Prognosis: Dynamic Risk Profiles
Once ARDS is established, knowing who is likely to deteriorate guides resource allocation and family counseling. Long short-term memory (LSTM) networks that ingest time series vitals and laboratory trends outperform conventional Sequential Organ Failure Assessment (SOFA) and Simplified Acute Physiology Score (SAPS II) tools; meta-analysis shows a concordance index of 0.84 versus 0.64–0.70 for traditional scores. By continuously updating risk, these models enable clinicians to decide when to escalate to extracorporeal membrane oxygenation (ECMO) or palliative pathways, rather than relying on “worst value in 24 hours” snapshots. However, the review cautions that most current models are focused on mortality risk, and broader outcome prediction (e.g., disability, quality of life) remains underexplored.
Phenotypes and Endotypes
Latent class analysis (LCA) applied to multicenter trial data revealed two reproducible inflammatory phenotypes: hyper-inflammatory, characterized by interleukin 6 surges and a 40–50% mortality rate, and hypo-inflammatory, associated with less organ failure and a roughly 20% mortality rate. Treatment responses diverge; high positive end-expiratory pressure (PEEP) harms the hyper-inflammatory group, yet may aid the hypo-inflammatory group. Supervised gradient boosting models now assign these phenotypes bedside using routine labs and vitals with an accuracy of 0.94–0.95, paving the way for phenotype-specific trials of corticosteroids, fluid strategies, or emerging biologics. The review also describes additional ARDS subtypes, such as those based on respiratory mechanics, radiology, or multi-omics data. It emphasizes that real-time bedside subtyping is a critical goal for future precision medicine.
Smarter Breathing Support
AI also refines everyday ventilation decisions. A multi-task neural network simulates how oxygenation and compliance will change 45 minutes after a PEEP adjustment, enabling virtual “test drives” instead of trial-and-error titration. Mechanical power (MP) is the energy delivered to the lung each minute and exceeds 12 Joules per minute in patients at the highest risk of ventilator-induced injury. XGBoost models individualize MP thresholds and predict ICU mortality with an AUC of 0.88. For patient-ventilator asynchrony (PVA), deep learning detectors sift through millions of breaths and achieve over 90% accuracy, promising real-time alarms or even closed-loop ventilators that self-correct harmful cycling. The review notes, however, that most PVA detection models remain offline, and real-time actionable systems are still in development.
High Stakes Decisions: ECMO and Liberation
ECMO can salvage gas exchange but consumes significant resources in terms of staffing and supplies. The hierarchical Prediction, Early Monitoring, and Proactive Triage for Extracorporeal Membrane Oxygenation (PreEMPT ECMO) deep network combines demographics, laboratory results, and minute-by-minute vital signs to forecast ECMO need up to 96 hours in advance (AUC = 0.89 at 48 hours), aiding in referral timing and equitable resource utilization. At the other end of the journey, AI-based systems are being explored to predict when ventilator weaning will succeed, shortening mechanical ventilation and hospital stay in proof-of-concept studies. However, the review highlights that most studies of AI for weaning and extubation are generally conducted in ICU populations, rather than ARDS-specific cohorts, and direct evidence in ARDS remains scarce. Integrating both tools could one day create a complete life cycle decision platform, but this remains an aspirational goal.
Next Generation Algorithms and Real World Barriers
Graph neural networks (GNNs) model relationships among patients, treatments, and physiologic variables, potentially uncovering hidden risk clusters. Federated learning (FL) trains shared models across hospitals without moving protected health data, improving generalizability. Self-supervised learning (SSL) leverages billions of unlabeled waveforms to pre-train robust representations. Large language models (LLMs) and emerging multimodal variants act as orchestrators, calling specialized image or waveform models and generating human-readable plans. The review additionally highlights causal inference and reinforcement learning (RL) as promising approaches for simulating “what-if” scenarios and for developing AI agents that make sequential decisions in dynamic ICU environments. These techniques promise richer insights but still face hurdles related to data quality, interpretability, and workflow integration that must be addressed before routine clinical adoption.
In the area of drug discovery, the review notes that while AI has enabled target and compound identification in related lung diseases (such as idiopathic pulmonary fibrosis), the application of generative AI for ARDS-specific therapies remains largely conceptual at present.
Conclusions
To summarize, current evidence shows that AI and ML can detect ARDS earlier, stratify risk more precisely, tailor ventilation to individual lung mechanics, and guide costly therapies such as ECMO. Phenotype-aware algorithms already flag patients who benefit from, or suffer from, high PEEP, while neural networks forecast MP-related injury and PVA in real-time. Next-generation GNNs, FL, RL, causal inference, and LLMs may weave disparate data into cohesive bedside recommendations. Rigorous prospective trials, transparent reporting, and clinician-friendly interfaces remain essential to translate these digital advances into lives saved and disabilities prevented.
Journal reference:
- Li S, Yue R, Lu S, Luo J, Wu X, Zhang Z, Liu M, Fan Y, Zhang Y, Pan C, Huang X and He H. (2025). Artificial intelligence and machine learning in acute respiratory distress syndrome management: recent advances. Front. Med. 12. DOI: 10.3389/fmed.2025.1597556 https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1597556/full




















You must be logged in to post a comment Login